Automated Prior Authorization Solution For Providers

Automated Prior Authorization Solution For Providers
Automated Prior Authorization Solution For Providers I've reviewed and evaluated the most popular prior authorization software and shortlisted the best ones to accelerate approvals and reduce administrative burdens. Explore 5 leading ai tools easing prior authorization. discover how healthcare providers save time, cut costs, and improve patient care efficiency.

Automated Prior Authorization | AI-Powered Solutions
Automated Prior Authorization | AI-Powered Solutions In this article, we explore the top 30 best prior authorization automation solutions helping providers enhance efficiency, minimize denials, and speed up access to care. Ai powered prior authorization solutions streamline the process of obtaining payer approvals for medical tests, procedures, and prescriptions. these solutions use machine learning, natural language processing (nlp), and automation to analyze patient data, insurance policies, and clinical guidelines. A comprehensive, intelligent platform solution and composable products to meet you and your providers where you are for scalable, long term success. 47% reduction in administrative cost powered by responsible, clinically derived ai and approval automation. Accelerate approvals with ai, automation and extensive payer integrations with patient access plus’ prior authorization module. navigating prior authorization processes can be tedious and time consuming, leading to delays in patient care and operational inefficiencies.

Automated Prior Authorization Software
Automated Prior Authorization Software A comprehensive, intelligent platform solution and composable products to meet you and your providers where you are for scalable, long term success. 47% reduction in administrative cost powered by responsible, clinically derived ai and approval automation. Accelerate approvals with ai, automation and extensive payer integrations with patient access plus’ prior authorization module. navigating prior authorization processes can be tedious and time consuming, leading to delays in patient care and operational inefficiencies. Myndshft automatically synchronizes eligibility and prior authorization rules to provide full transparency for providers and patients. Klinic offers expert prior authorization services for medications, providing outsourced solutions for providers to ensure faster approvals and reduced burden. Informatics in context’s (iic) offers payers a transformative standards based solution which fully automates their prior authorization (pa) process in real time based on the aca mandated edi 278 standard for medical procedures, tests, labs, and drugs covered under medical benefits. Janus health makes prior authorizations faster and easier by automating the whole process—determining if it’s needed, starting the request, and checking the status—all in real time. we integrate directly with your ehr so staff can work in the systems they already use.

Automated Prior Authorization With AI
Automated Prior Authorization With AI Myndshft automatically synchronizes eligibility and prior authorization rules to provide full transparency for providers and patients. Klinic offers expert prior authorization services for medications, providing outsourced solutions for providers to ensure faster approvals and reduced burden. Informatics in context’s (iic) offers payers a transformative standards based solution which fully automates their prior authorization (pa) process in real time based on the aca mandated edi 278 standard for medical procedures, tests, labs, and drugs covered under medical benefits. Janus health makes prior authorizations faster and easier by automating the whole process—determining if it’s needed, starting the request, and checking the status—all in real time. we integrate directly with your ehr so staff can work in the systems they already use.

Automated Prior Authorization Solutions
Automated Prior Authorization Solutions Informatics in context’s (iic) offers payers a transformative standards based solution which fully automates their prior authorization (pa) process in real time based on the aca mandated edi 278 standard for medical procedures, tests, labs, and drugs covered under medical benefits. Janus health makes prior authorizations faster and easier by automating the whole process—determining if it’s needed, starting the request, and checking the status—all in real time. we integrate directly with your ehr so staff can work in the systems they already use.

Automated Prior Authorization With Intelligent Automation - Nividous Intelligent Automation Company
Automated Prior Authorization With Intelligent Automation - Nividous Intelligent Automation Company
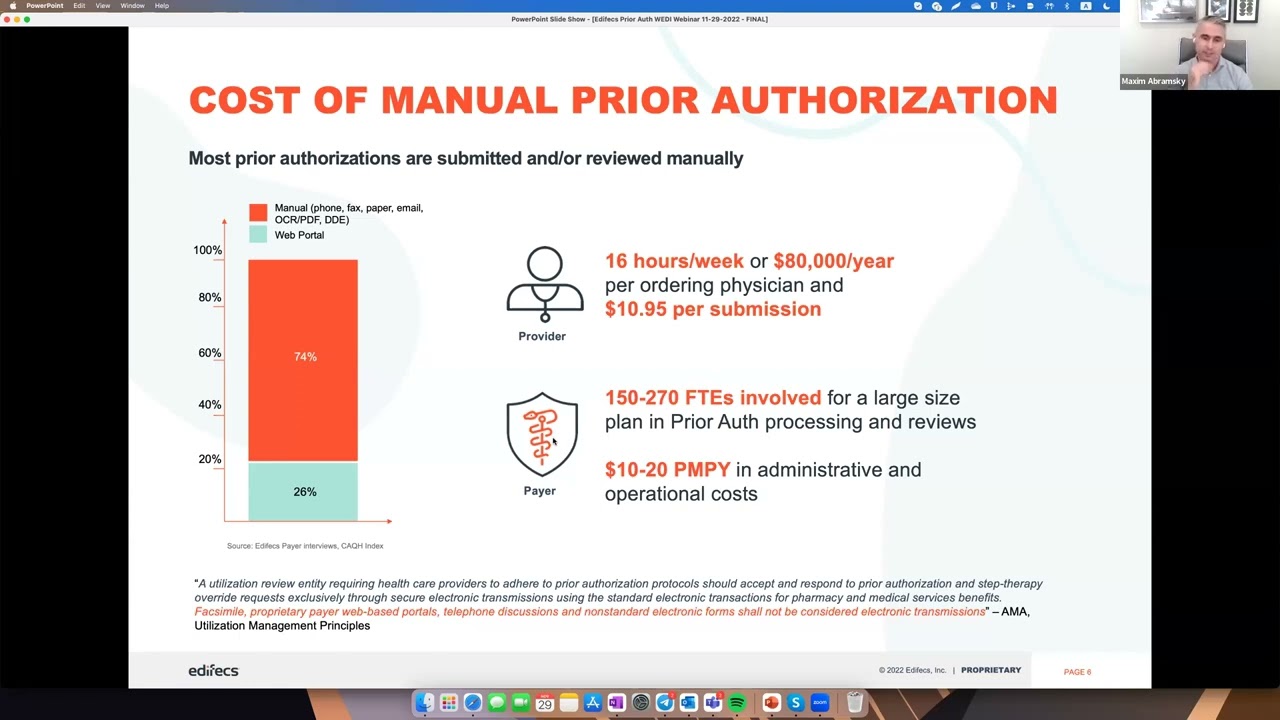
Automated Prior Authorization in Real Time for Payers & Providers. Presented by Edifecs
Automated Prior Authorization in Real Time for Payers & Providers. Presented by Edifecs
Related image with automated prior authorization solution for providers
Related image with automated prior authorization solution for providers
About "Automated Prior Authorization Solution For Providers"
















Comments are closed.